- Research
- Open access
- Published:
Implementing spiritual care education into the teaching of palliative medicine: an outcome evaluation
BMC Medical Education volume 24, Article number: 411 (2024)
Abstract
Background
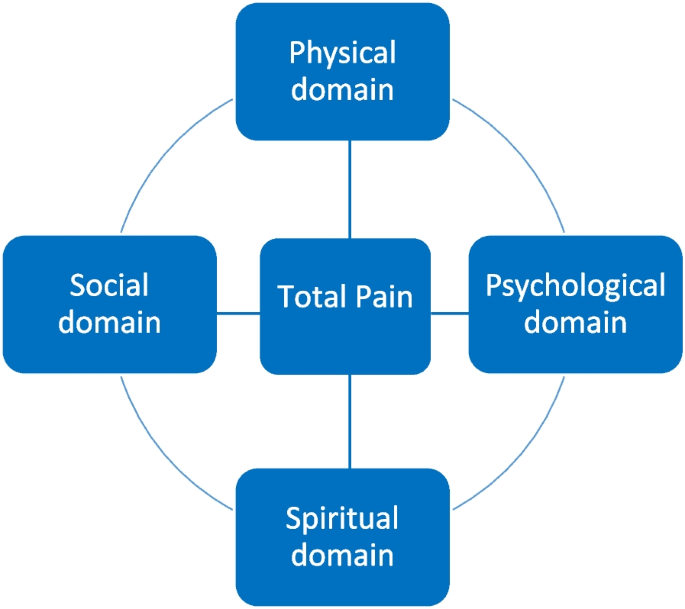
The concept of “total pain” plays an important role in palliative care; it means that pain is not solely experienced on a physical level, but also within a psychological, social and spiritual dimension. Understanding what spirituality entails, however, is a challenge for health care professionals, as is screening for the spiritual needs of patients.
Objective
This is a novel, interprofessional approach in teaching undergraduate medical students about spiritual care in the format of a seminar. The aim of this study is to assess if an increase in knowledge about spiritual care in the clinical context is achievable with this format.
Methods
In a mandatory seminar within the palliative care curriculum at our university, both a physician and a hospital chaplain teach strategies in symptom control from different perspectives (somatic domain – spiritual domain). For evaluation purposes of the content taught on the spiritual domain, we conducted a questionnaire consisting of two parts: specific outcome evaluation making use of the comparative self-assessment (CSA) gain and overall perception of the seminar using Likert scale.
Results
In total, 52 students participated. Regarding specific outcome evaluation, the greatest gain was achieved in the ability to define total pain (84.8%) and in realizing its relevance in clinical settings (77.4%). The lowest, but still fairly high improvement was achieved in the ability to identify patients who might benefit from spiritual counselling (60.9%). The learning benefits were all significant as confirmed by confidence intervals. Overall, students were satisfied with the structure of the seminar. The content was delivered clearly and comprehensibly reaching a mean score of 4.3 on Likert scale (4 = agree). The content was perceived as overall relevant to the later work in medicine (mean 4.3). Most students do not opt for a seminar solely revolving around spiritual care (mean 2.6).
Conclusions
We conclude that implementing spiritual care education following an interprofessional approach into existing medical curricula, e.g. palliative medicine, is feasible and well perceived among medical students. Students do not wish for a seminar which solely revolves around spiritual care but prefer a close link to clinical practice and strategies.
Introduction
Education in palliative care was introduced in 2009 as a compulsory subject in German medical curricula. In the 1960s, Dame Cicely Saunders established palliative medicine and hospices as we know them today. Back then, Cicely Saunders propagated the concept of “total pain”, which means that pain or suffering in general is not solely experienced on a physical level, but also within a psychological, social and spiritual dimension (see. Fig. 1) [1,2,3,4]. Understanding the importance of spirituality in everyday clinical practice and what it entails, however, is a challenge for health care professionals (HCP) in all medical disciplines across the world [5, 6]. Palliative care is a relatively young medical discipline which oftentimes is not sufficiently taught in medical curricula [1, 7] and, therefore, knowledge regarding the importance of spirituality, which at many faculties is integrated into palliative care education, is scarce [1, 7]. As a result, HCP tend to neglect the spiritual needs of patients [7, 8]. But, if there is no fundamental knowledge in regards of spirituality and spiritual care among physicians, how can they target total pain adequately?
The European Association of palliative care (EAPC) describes spirituality as following:
It must be clear to all HCP that spirituality is a unique and subjective phenomenon that differs substantially from patient to patient [2, 10]. Furthermore, to fully address the spiritual needs of patients, self-reflection, thorough consideration of one’s own attitude towards death, and finding meaning in life, are essential [8, 9]. Several studies have shown the impact which the addressing of spiritual needs in the context of total pain can have on ameliorating the symptoms of patients, leading to a better quality of life and care [11,12,13,14,15,16,17,18]. Thus, once spiritual needs become imminent, it is necessary to engage in an interdisciplinary and multi-professional collaboration with specially trained professionals in the field of spiritual care [8, 10, 14, 15, 19]. Summing up, it is very important to raise awareness about the positive impact of spiritual care among HCPs [8, 15]. To increase such knowledge and accrue such skills, the teaching of spiritual care in medical curricula is essential [20]. Throughout different regions in the world, in-person didactic teaching on spiritual care is the most commonly used technique [5]. Usually, the teaching is based on case studies and many include screening strategies assessing spiritual needs [5]. Often, education on spirituality and spiritual care is part of curricula in palliative care [5, 21]. In German medical curricula, there is no compulsory subject solely revolving around spiritual care [22]. However, regarding the concept of total pain, implementing spiritual care into palliative care teaching, however, seems like a plausible proposition.
This study was conducted in order to assess the way medical students perceive the concept of implementing spiritual care into the teaching on symptom control in palliative care. Furthermore, we aimed to determine whether an actual increase of knowledge about spiritual care in the clinical context was achievable within this seminar.
Material and methods
This study is a single-centre prospective study conducted at University Hospital Duesseldorf, Germany. Ethical approval was obtained by the local ethics committee (reference number 2022–2274).
Curricular structure
At our facility, palliative care education is structured as followed: Five lectures (somatic symptoms, psychological symptoms, social symptoms and advance care planning, spiritual symptoms and end-of-life care and care for relatives, clinical ethics) and four seminars (symptom control, breaking bad news, clinical ethics I and II). Since 2022, the lecture on spiritual symptoms and end-of-life-care is held by both a physician and a hospital chaplain within the palliative care curriculum at Düsseldorf medical faculty. Beforehand, this lecture was solely held by a hospital chaplain. As internal evaluations implied, this concept was not well perceived by medical students as the relevance to daily clinical work was not apparent to them. They did not understand how spiritual care can support somatic strategies of symptom control and how both approaches are intertwined. Furthermore, they were unsure of how to assess patients’ spiritual needs. We therefore opted for the above-mentioned approach which allows lecturing relevant medical implications alongside spiritual care. As evaluations showed, this embeds spiritual care in a more clinical and tangible manner and students seem to better realize the relevance that spiritual care has in daily clinical practice. For example, students repeatedly stated that they were now able to understand the importance of ongoing collaborations for patients’ comfort care, e.g., in more sufficiently relieving anxiety or social distress.
Since this novel concept was perceived positively by medical students, we transposed it to our seminar titled “symptom control” which is now also held by a hospital chaplain and a physician. In the seminars, content from the lectures is further deepened and there is more room for discussions, e.g. concerning assessment of spiritual needs, possibilities of spiritual care, and inter-professional collaboration. There is also an emphasis on determining which patients might benefit from spiritual care making use of the SPIR tool (patient’s self-description as a Spiritual person—Place of spirituality in patient’s life – patient’s Integration in a spiritual community – Role of health care professional in the domain of spirituality), which tackles different dimensions of spirituality [23].
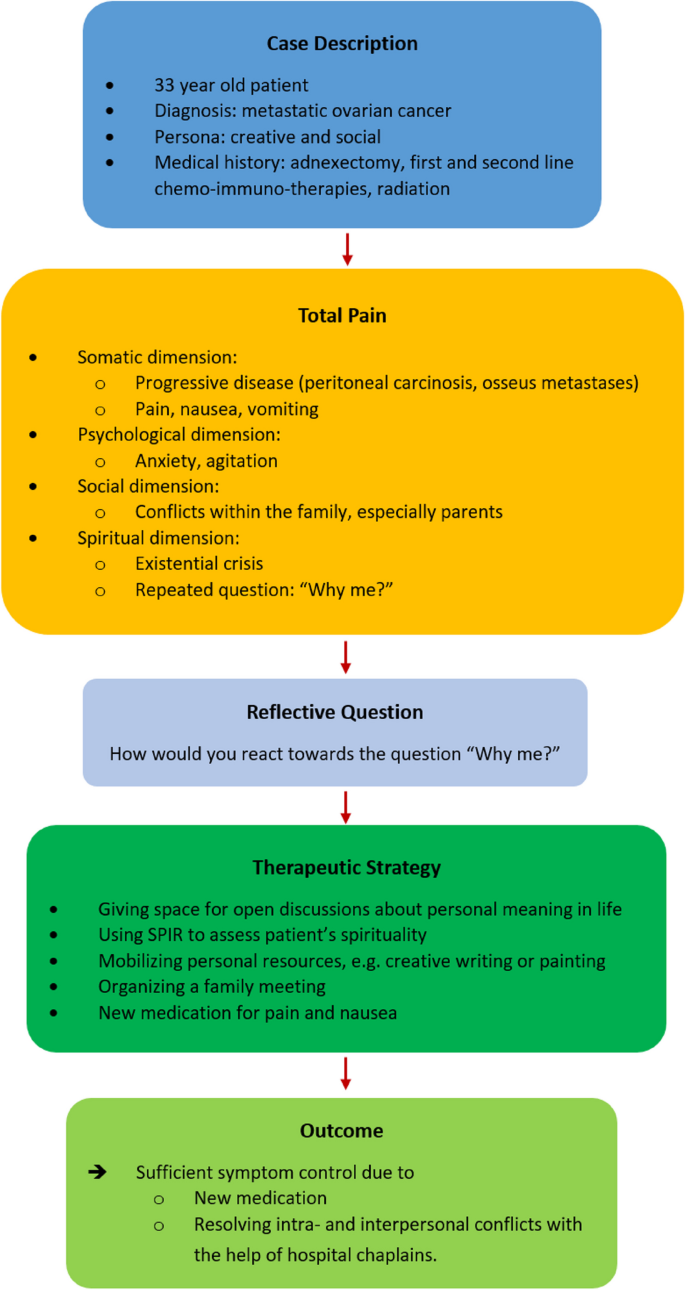
In the seminar, a 33-year-old fictitious patient (inspired by a real patient) served as an example case. Her situation is used to address strategies for symptom control on both somatic and spiritual domains. To achieve this, a reflective question is discussed with the students followed by a joint development of possible therapeutic strategies on both the somatic and spiritual domain (see Fig. 2).
Our approach can be described as novel, since training in spiritual care often involves the mere shadowing of chaplains [5, 24,25,26]. An interprofessional, educational approach was mainly used with physicians or nurses in training [5, 27,28,29], but not with medical students.
Evaluation methods
A structured, paper-based questionnaire was developed in repeated interdisciplinary and multi-professional discussions in the Interdisciplinary Centre for Palliative Care Medicine, University Hospital Düsseldorf, Germany. The basis for the questionnaire were the learning goals that are to be achieved within the seminar, as well as a didactic evaluation. The questionnaire was pretested among medical students, and unclear statements were altered. The questionnaire consists of two parts. The first part is made up of five statements regarding knowledge about total pain, assessing spiritual needs, and defining spiritual care (see Table 1) on both the knowledge and skills level. These statements cover the field of specific outcome evaluation. Making use of the comparative self-assessment (CSA) method to determine if a gain in knowledge was achieved, each student evaluated their knowledge before and after the seminar using the German school grading system (1 = “excellent” to 6 = “unsatisfactory”). The CSA gain is a well described and implemented method in evaluating actual knowledge gains in education [30,31,32,33,34]. This evaluation tool has the benefit of not taking into account experiences made beforehand as they are not contributing to the effect size [31]. CSA gain is calculated as followed:
Furthermore, CSA gain was calculated with a 95% confidence interval and standard error using individual learning gain (ILG) values. These values were calculated using the following formulas:
-
ILG = 0 if pre = post and
-
ILG = (pre − post)/(pre − 1) × 100 if pre > post [31].
The second part of the questionnaire consists of four questions regarding the perception of the seminar (structure, teaching spiritual care alongside symptom control in palliative care). A 5-Point-Likert scale was used for evaluation (1 = strongly disagree, 2 = disagree, 3 = neither, 4 = agree, 5 = strongly agree).
Study participation and analysis
Participation in the study was anonymous, voluntary, and could be withdrawn at any time without explanation. Eligible participants were undergraduate medical students at the beginning of their fifth year of medical education (Germany: total of min. six years), who completed the mandatory palliative care course. The purpose and content of the study were presented orally, and, furthermore, written information and consent documents were handed out. After completion of the seminar, the questionnaire was handed out making use of a post-then design in which the students were asked to retrospectively rate their knowledge before and after the seminar. There were no exclusion criteria other than refusing to participate. Due to the small number of students per seminar (n = 15–20), no demographic characteristics besides sex were assessed.
Data analysis was performed using Microsoft Excel 2020 (version 16.42, Microsoft Corp., Redmond, WA, USA) and IBM SPSS Statistic version 28.0.1.1 (IBM, Armonk, NY, USA).
Results
Throughout the course of one semester in 2023, the questionnaires were rolled out in each of six separate seminars. Out of 108 eligible attending students, 52 students participated in total (48.1%). 25% (n = 13) of the participants were of female, 75% (n = 39) of male sex. Within the answered questionnaires, there was no missing data.
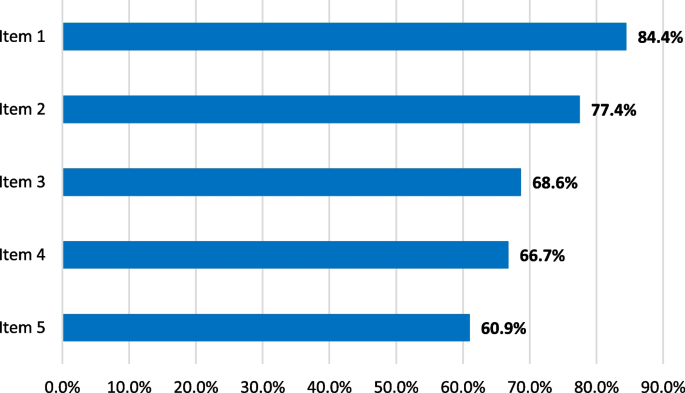
Regarding the specific outcome evaluation, CSA gains showed a relevant increase especially in the field of knowledge (see Table 2 and Fig. 3). The greatest improvement (84.8%) was achieved in the ability of defining total pain and realizing its importance in clinical settings (77.4%). After the seminar, medical students were increasingly able to name tools such as SPIR in order to engage in spiritual needs assessment (CSA gain 68,8%). A lower increase in knowledge was achieved in realizing how spiritual care itself can benefit patients’ needs (66.7%). The lowest gain was detected in actually identifying patients who might benefit from spiritual care (60.9%), which represents a skill to be learned rather than knowledge to be gained.
Statistical analysis using 95% confidence intervals confirmed the gains in knowledge, which were significant for all items (Table 2).
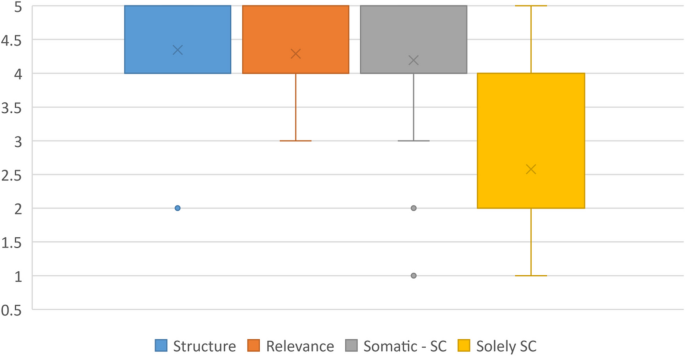
In regard to the second part of the questionnaire, students were overall satisfied with the new structure of the seminar (Table 3 and Fig. 4). The content was comprehensible and delivered clearly gaining a mean score of 4.3 (median 4, SD 0.6, min. 2, max. 5). The content was perceived as overall relevant to the later work in medicine (mean 4.3, median 4, SD 0.6, min. 3, max. 5). It seems as if medical students regard the implementation of spiritual care education into the seminar “symptom control”, which focuses on alleviating symptoms on multidimensional levels, as expedient. They feel that implementing education on spiritual care into this seminar makes sense (mean 4.2, median 4, SD 0.8, min. 1, max. 5). Furthermore, most students do not opt for a seminar solely revolving around spiritual care (mean 2.6, median 2, SD 1.3, min. 1, max. 5).
Discussion
Our data show that implementing spiritual care education into existing medical curricula, in our example palliative care, is feasible and well perceived among medical students. The timing of our seminar is in accordance to other studies that found that spiritual care should be implemented in mandatory undergraduate courses [6]. Students do not wish for a seminar solely revolving around spiritual care but prefer a connection to clinical practice and strategies in symptom management. This enables them to understand the relevance of spiritual care in a daily clinical setting.
To evaluate training programs, Kirkpatrick proposed a four-level approach (level 1: reaction, level 2: learning, level 3: behaviour, level 4: results) [35]. We followed levels 1 (reaction—satisfaction) and 2 (learning—gains in knowledge) making use of the conducted questionnaire. Level 3 (change in behaviour – acquired skills) was briefly addressed with item 5 in the first part of the questionnaire. As level 4 is an indicator of direct results of the training at an organizational level, we were not able to incorporate items on this level. A different study among undergraduate nursing students assessed the effectiveness of teaching spiritual care in mandatory classes: There was an increase in knowledge, e.g., in defining spirituality, compared to students who obtained no information on spiritual care [36]. This is comparable to our study, as there were gains in knowledge after completing the mandatory seminar. We reached higher individual learning gains on the knowledge level than on the skills level, as was also the case in a number of other studies we conducted [31]. This is mainly because, due to the format of the seminar, no bedside teaching takes place and scenarios that might occur in everyday clinical practice can only be discussed and serve as examples.
The concept of total pain is essential in palliative care; however, it should not only be taken into consideration in a palliative setting, but whenever patients experience high burdens on various dimensions such as pain, anxiety, grief or existential distress [2, 4, 17, 37, 38]. We were able to thoroughly educate students on total pain and its relevance in clinical settings. Spirituality plays an important role in a holistic approach. However, literature shows that HCP often don’t know how to implement spiritual assessments and how to deal with spiritual needs [1, 5, 6, 8]. A systematic review on teaching methods found the usage of practical tools and the involvement of chaplains to be effective facilitators in the teaching of spiritual care [5]. A scoping review found that spiritual care should be taught in both mono- and multi-disciplinary educational settings [6]. With our multi-professional approach, we were able to introduce students to tools in assessing spiritual needs, such as SPIR [23]. Within this item, there was a definite gain in knowledge of these tools which make assessing spiritual needs of patients more feasible. This is in accordance with findings of a number other studies [5]. In our study, however, students are still unsure if they are fully able to determine which patients might actually benefit from spiritual care, even though this item still reached a learning gain of 60.9%. As concluded by other authors, there is need for ongoing education [5].
Even though our seminar entails many different aspects of the total pain concept (somatic symptom management, spirituality, and spiritual care) medical students found the content to be clearly structured and comprehensible. More importantly, they understood the relevance of spirituality for their future clinical work and perceived the multi-professional teaching as highly satisfactory. In sensitizing them in this, we hope that they keep in mind the importance of ongoing collaborations between different professions.
Our study has some limitations. Even though the questionnaire was pretested among medical students before the actual study, no validated questionnaire was used. The response rate of almost 50% is relatively low and it can be assumed that those who participated were mostly students who were interested in the topic. This might have led to bias as positive effects might have been overestimated. Due to the small study population and to protect the privacy of participating students, no demographic data besides sex was collected. Demographic data, however, might contribute to a better understanding of spirituality or palliative medicine beforehand such as age, professional expertise, or own spiritual resources. This also meant that adjusting for confounding factors was not possible. This study solely dealt with medical students and no patients were involved. It would be of interest to assess as to whether the content taught in this seminar ultimately impacts the wellbeing or stress levels of patients in everyday clinical practice. A study focusing on patients would complement the findings of this study, as suggested by other researchers [5]. Furthermore, the study was only performed in one centre; therefore, it can only serve as an example on how spiritual care education might be successfully implemented into medical curricula.
Conclusions
Spirituality plays an important role for many people and should always be taken into consideration when treating patients. This especially applies to palliative care where the addressing of spiritual needs is of crucial importance [18]. However, many HCP don’t know how to address topics revolving around spirituality which makes it hard to determine which patients might benefit from spiritual care. Therefore, education on the nature of spiritual care, on what it entails and on how it can support patients in everyday clinical practice should be thoroughly integrated into medical curricula. We opted to implement spirituality and spiritual care into an existing seminar and lecture within the medical curriculum at our faculty. This was well received among students. As a result, we found a clear increase in knowledge about total pain and about the tools one might use to assess spiritual needs. This knowledge needs to be further strengthened in practical clinical scenarios.
Availability of data and materials
All data and materials are available within this publication.
Abbreviations
- HCP:
-
Health care professional
- EAPC:
-
European Association of palliative care
- SC:
-
Spiritual care
References
Best M, Leget C, Goodhead A, Paal P. An EAPC white paper on multi-disciplinary education for spiritual care in palliative care. BMC Palliat Care. 2020;19(1):9.
Goebel JR, Doering LV, Lorenz KA, Maliski SL, Nyamathi AM, Evangelista LS. Caring for special populations: total pain theory in advanced heart failure: applications to research and practice. Nurs Forum (Auckl). 2009;44(3):175–85.
Krok D, Telka E, Zarzycka B. Total Pain and Illness Acceptance in Pelvic Cancer Patients: Exploring Self-Efficacy and Stress in a Moderated Mediation Model. Int J Environ Res Public Health. 2022;19(15):9631.
Rettke H, Naef R, Rufer M, Peng-Keller S. Spirituality and health care. The perspective of patients with chronic pain. Schmerz. 2021;35(5):333–42.
Jones KF, Paal P, Symons X, Best MC. The Content, Teaching Methods and Effectiveness of Spiritual Care Training for Healthcare Professionals: A Mixed-Methods Systematic Review. J Pain Symptom Manage. 2021;62(3):e261–78.
Rykkje L, Søvik MB, Ross L, McSherry W, Cone P, Giske T. Educational interventions and strategies for spiritual care in nursing and healthcare students and staff: A scoping review. J Clin Nurs. 2022;31(11–12):1440–64.
Puchalski CM, Sbrana A, Ferrell B, Jafari N, King S, Balboni T, et al. Interprofessional spiritual care in oncology: A literature review, vol. 4. ESMO Open: BMJ Publishing Group; 2019.
Willemse S, Smeets W, van Leeuwen E, Nielen-Rosier T, Janssen L, Foudraine N. Spiritual care in the intensive care unit: An integrative literature research. J Crit Care. 2020;1(57):55–78.
Chahrour WH, Hvidt NC, Hvidt EA, Viftrup DT. Learning to care for the spirit of dying patients: the impact of spiritual care training in a hospice-setting. BMC Palliat Care. 2021;20(1):115.
Gomes-Ferraz CA, Rezende G, Fagundes AA, De Carlo MMR do P. Assessment of total pain in people in oncologic palliative care: integrative literature review. Palliat Care Soc Pract. 2022;16:26323524221125244 SAGE Publications Ltd.
Evangelista CB, Lopes MEL, Costa SFG da, Batista PS de S, Batista JBV, Oliveira AM de M. Palliative care and spirituality: an integrative literature review. Rev Bras Enferm. 2016;69(3):591–601.
Gijsberts MJHE, Liefbroer AI, Otten R, Olsman E. Spiritual Care in Palliative Care: A Systematic Review of the Recent European Literature. Medical Sciences. 2019;7(2):25.
Bai J, Brubaker A, Meghani SH, Bruner DW, Yeager KA. Spirituality and Quality of Life in Black Patients With Cancer Pain. J Pain Symptom Manage. 2018;56(3):390–8.
Grossoehme DH, Friebert S, Baker JN, Tweddle M, Needle J, Chrastek J, et al. Association of Religious and Spiritual Factors With Patient-Reported Outcomes of Anxiety, Depressive Symptoms, Fatigue, and Pain Interference Among Adolescents and Young Adults With Cancer. JAMA Netw Open. 2020;3(6): e206696.
Klop HT, Koper I, Schweitzer BPM, Jongen E, Onwuteaka-Philipsen BD. Strengthening the spiritual domain in palliative care through a listening consultation service by spiritual caregivers in Dutch PaTz-groups: An evaluation study. BMC Palliat Care. 2020;19(1):92.
Phenwan T. Relieving total pain in an adolescent: A case report. BMC Res Notes. 2018;11(1):265.
Wisesrith W, Sukcharoen P, Sripinkaew K. Spiritual Care Needs of Terminal Ill Cancer Patients. Asian Pac J Cancer Prev. 2021;22(12):3773–9.
Fegg MJ, Brandstätter M, Kramer M, Kögler M, Haarmann-Doetkotte S, Borasio GD. Meaning in Life in Palliative Care Patients. J Pain Symptom Manage. 2010;40(4):502–9.
Arrieira IC de O, Thofehrn MB, Porto AR, Moura PMM, Martins CL, Jacondino MB. Spirituality in palliative care: Experiences of an interdisciplinary team. Revista da Escola de Enfermagem. 2018;52:e03312.
Pieters J, Dolmans DHJM, Verstegen DML, Warmenhoven FC, Courtens AM, Van Den Beuken-Van Everdingen MHJ. Palliative care education in the undergraduate medical curricula: Students’ views on the importance of, their confidence in, and knowledge of palliative care. BMC Palliat Care. 2019;18(1):72.
Paal P, Roser T, Frick E. Developments in spiritual care education in German - Speaking countries. BMC Med Educ. 2014;14(1):112.
MFT Medizinischer Fakultätentag der Bundesrepublik Deutschland e.V., editor Nationaler Kompetenzbasierter Lernzielkatalog Medizin (NKLM) [Internet]. 2015 [cited 2024 Mar 11]. Available from: http://www.nklm.de/
Frick E, Riedner C, Fegg M, Hauf S, Borasio G. A clinical interview assessing cancer patients’ spiritual needs and preferences. Eur J Cancer Care (Engl). 2006;15:238–43.
Gomez S, White B, Browning J, DeLisser HM. Medical Students’ Experience in a Trauma Chaplain Shadowing Program: A Mixed Method Analysis. Med Educ Online. 2020;25(1):1710896.
Bell D, Harbinson M, Toman G, Crawford V, Cunningham H. Wholeness of Healing: An Innovative Student-Selected Component Introducing United Kingdom Medical Students to the Spiritual Dimension in Healthcare. South Med J. 2010;103(12):1204–9.
Hemming P, Teague PJ, Crowe T, Levine R. Chaplains on the Medical Team: A Qualitative Analysis of an Interprofessional Curriculum for Internal Medicine Residents and Chaplain Interns. J Relig Health. 2016;55(2):560–71.
Robinson MR, Thiel MM, Shirkey K, Zurakowski D, Meyer EC. Efficacy of Training Interprofessional Spiritual Care Generalists. J Palliat Med. 2016;19(8):814–21.
Huehn SL, Kuehn MB, Fick KE. Integrating Spiritual Care During Interprofessional Simulation for Baccalaureate Nursing Students. J Holist Nurs. 2019;37(1):94–9.
Anandarajah G, Roseman J, Lee D, Dhandhania N. A 10-Year Longitudinal Study of Effects of a Multifaceted Residency Spiritual Care Curriculum: Clinical Ability, Professional Formation, End of Life, and Culture. J Pain Symptom Manage. 2016;52(6):859-872.e1.
Raupach T, Münscher C, Beißbarth T, Burckhardt G, Pukrop T. Towards outcome-based programme evaluation: Using student comparative self-assessments to determine teaching effectiveness. Med Teach. 2011;33(8):e446-53.
Schwartz J, Schallenburger M, Tenge T, Batzler YN, Schlieper D, Kindgen-Milles D, et al. Palliative Care e-Learning for Physicians Caring for Critically Ill and Dying Patients during the COVID-19 Pandemic: An Outcome Evaluation with Self-Assessed Knowledge and Attitude. Int J Environ Res Public Health. 2022;19(19):12377.
Laupichler MC, Hadizadeh DR, Wintergerst MWM, von der Emde L, Paech D, Dick EA, et al. Effect of a flipped classroom course to foster medical students’ AI literacy with a focus on medical imaging: a single group pre-and post-test study. BMC Med Educ. 2022;22(1):803.
Thyson T, Schallenburger M, Scherg A, Leister A, Schwartz J, Neukirchen M. Communication in the face of death and dying - how does the encounter with death influence the patient management competence of medical students? An outcome-evaluation. BMC Med Educ. 2022;22(1):25.
Seifert T, Becker T, Büttcher AF, Herwig N, Raupach T. Restructuring the clinical curriculum at University Medical Center Göttingen: effects of distance teaching on students’ satisfaction and learning outcome. GMS J Med Educ. 2021;38(1):Doc1.
Kirkpatrick DL. Evaluating Training Programs. San Francisco, CA, USA: Berret-Koehler Publishers, Inc.; 1994.
Yilmaz M, Gurler H. The efficacy of integrating spirituality into undergraduate nursing curricula. Nurs Ethics. 2014;21(8):929–45.
Faria C, Branco V, Ferreira P, Gouveia C, Trevas S. Total Pain Management and a Malignant Wound: The Importance of Early Palliative Care Referral. Cureus. 2021;13(12):e20678.
Best M, Aldridge L, Butow P, Olver I, Webster F. Conceptual analysis of suffering in cancer: a systematic review. Psychooncology. 2015;24(9):977–86.
Acknowledgements
We thank Dr Jessica JT Fischer for excellent English language editing.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YB, NS, MS, JS, MN designed the study. YB analysed and interpreted the data. YB drafted the first version of the manuscript, which was critically revised by NS, MS, JS, and MN in several rounds of feedback. All authors have approved the submitted version and have agreed to be accountable for their contributions as well as for accuracy and integrity for any part of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Committee of Heinrich-Heine-University Düsseldorf (Study No. 2022–2274). Written informed consent was obtained from all participants, which were all over 18 years and informed about the study before starting the questionnaire. Researchers assured participants that the contents of the surveys would be used solely for research purposes.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Heinrich Heine University Duesseldorf (reference number 2022-2274).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Batzler, YN., Stricker, N., Bakus, S. et al. Implementing spiritual care education into the teaching of palliative medicine: an outcome evaluation. BMC Med Educ 24, 411 (2024). https://doi.org/10.1186/s12909-024-05415-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05415-0