- Research
- Open access
- Published:
Complex interplay of neurodevelopmental disorders (NDDs), fractures, and osteoporosis: a mendelian randomization study
BMC Psychiatry volume 24, Article number: 232 (2024)
Abstract
Background
Neurodevelopmental disorders (NDDs), such as Attention-Deficit/Hyperactivity Disorder (ADHD), Autism Spectrum Disorder (ASD), and Tourette Syndrome (TS), have been extensively studied for their multifaceted impacts on social and emotional well-being. Recently, there has been growing interest in their potential relationship with fracture risks in adulthood. This study aims to explore the associations between these disorders and fracture rates, in order to facilitate better prevention and treatment.
Methods
Employing a novel approach, this study utilized Mendelian randomization (MR) analysis to investigate the complex interplay between ADHD, ASD, TS, and fractures. The MR framework, leveraging extensive genomic datasets, facilitated a systematic examination of potential causal relationships and genetic predispositions.
Results
The findings unveil intriguing bidirectional causal links between ADHD, ASD, and specific types of fractures. Notably, ADHD is identified as a risk factor for fractures, with pronounced associations in various anatomical regions, including the skull, trunk, and lower limbs. Conversely, individuals with specific fractures, notably those affecting the femur and lumbar spine, exhibit an increased genetic predisposition to ADHD and ASD. In this research, no correlation was found between TS and fractures, or osteoporosis.These results provide a genetic perspective on the complex relationships between NDDs and fractures, emphasizing the importance of early diagnosis, intervention, and a holistic approach to healthcare.
Conclusion
This research sheds new light on the intricate connections between NDDs and fractures, offering valuable insights into potential risk factors and causal links. The bidirectional causal relationships between ADHD, ASD, and specific fractures highlight the need for comprehensive clinical approaches that consider both NDDs and physical well-being.
Introduction
Attention Deficit Hyperactivity Disorder (ADHD), Autism Spectrum Disorder (ASD), and Tourette Syndrome (TS) are prominent Neurodevelopmental disorders(NDDs)often co-occurring and impactingsocial and emotional aspects [1]. Observational studies reveal higher fracture risks among adults with these conditions compared to those without [2]. Notably, ADHD is associated with an increased risk of fractures, highlighting the importance of recognizing the elevated risk in individuals with ADHD [3,4,5,6].
The core features of ADHD involve attention deficits, heightened hyperactivity, and impulsive behaviors. Notably, children with ADHD face an elevated risk of fractures, particularly affecting the skull, neck, trunk, and intracranial structures, with a Hazard Ratio (HR) 3.07 times higher than neurotypical peers [7]. Research highlights the statistical significance (P < 0.001) of this heightened fracture risk, encompassing regions such as the skull, neck, and trunk (HR = 1.53), upper limbs (HR = 1.28), and lower extremities (HR = 1.84) [5]. Moreover, studies indicate a correlation between ADHD symptoms and limb fractures in adults [8], with a notable reduction in fracture risk for individuals receiving pharmacological interventions [9, 10].
ASD is a NDDs by social impairment and restricted interactive and communicative behaviors [11]. Notably, individuals within the ASD spectrum exhibit an increased susceptibility to injuries involving the head, face, and neck [12], as well as a heightened risk of fractures affecting the hip, forearm, and spine [13]. Additionally, adolescent boys with ASD display lower bone mineral density (BMD) in comparison to their neurotypical peers [14].
Research consistently reveals distinctive patterns in bone health among individuals with ASD, including reduced systemic bone mineral content, diminished cortical area, and thinning of cortical and trabecular bone structures, especially in the distal radius and tibia. These trends extend to various anatomical regions, such as the lumbar spine, hips, and femoral neck, setting individuals with ASD apart from those without the condition [15].
TS is an intricate NDDs characterized by the presence of persistent vocal and motor tics, a defining feature that must endure for at least one year. Notably, a comprehensive decade-long cohort study unveiled a 1.27-fold higher fracture rate in individuals within the TS cohort when compared to a meticulously matched control cohort. Furthermore, a thorough multivariate Cox regression analysis revealed an adjusted HR of 1.28. Of particular interest is the observation that the introduction of antipsychotic medications led to a notable reduction in this heightened risk, resulting in a decreased HR of 1.17 [16]. This phenomenon warrants investigation, considering factors such as self-harm, accidental injuries, and the potential consequences of antipsychotic medication-related side effects [16, 17].
Fractures and osteoporosis cast a significant shadow over public health [18], with a disquieting projection of over 30 million individuals expected to be affected by bone-related conditions in Europe by the year 2050. The associated financial burden is equally disconcerting, with potential hospitalization costs in Europe alone estimated to reach up to €3.5 billion annually [19]. It is crucial to acknowledge that while genetics play a substantial role, one’s bone structure is subject to modification, influenced by intrinsic and extrinsic factors such as physical activity, hormonal dynamics, and nutritional status [20].
The pivotal role of nutrition and physical activity takes center stage in strengthening bones during crucial early developmental stages. This emphasis on early intervention stems from the understanding that as individuals progress through life, the gradual accrual of undesirable bone mass can lead to bone fragility and, ultimately, the onset of osteoporosis. Aligned with the insights of the International Osteoporosis Foundation, osteoporosis is aptly defined as a condition characterized by low bone mass and the progressive deterioration of bone microstructure, culminating in heightened bone fragility and an elevated risk of fractures [21].
Fractures in the Pediatric and Adolescent Realm: A Significant Component of Injuries:
Fractures hold a significant place in the realm of accidents and injuries, accounting for a substantial 25% of all such incidents involving children and adolescents. While a wide array of risk factors has been identified, including factors like nutritional deficiencies [22], high body weight, and intense physical activities [23], as well as psychiatric disorders such as schizophrenia [24], the intricate interplay between fractures, osteoporosis, and the three NDDs of ADHD, ASD, and TS warrants comprehensive examination.
Simultaneously, cross-disease investigations have uncovered significant overlap in the phenotypic traits associated with the genetic risk shared by ADHD, ASD, and TS [1]. Grounded in the characteristic features of inattention, hyperactivity, and impulsivity commonly observed in individuals with ADHD, previous research provides a compelling basis for postulating causal links between ADHD, ASD, TS and the occurrence of fractures and osteoporosis. Furthermore, considering the associations among ADHD, ASD, TS, and intellectual disabilities, all of which fall within the spectrum of NDDs [25, 26], we have deliberately incorporated intellectual functioning into the scope of our investigation to enhance the credibility of our research. It is essential to recognize that these causal relationships may exhibit distinct patterns across various anatomical sites.
Mendelian randomization (MR) methodologies harness the potential of single nucleotide polymorphisms (SNPs) as instrumental variables(IVs) to rigorously estimate the causal relationships between exposures and specific outcomes. This approach offers a distinct advantage by significantly mitigating the impact of confounding variables and measurement errors that often confound traditional multivariate regression models [27]. Moreover, the deliberate exclusion of IVs that overlap with confounding factors in MR analyses minimizes the risk of bias, thereby enhancing the validity of causal inferences [28].
Our primary aim is to utilize the robust MR methodology for a comprehensive evaluation of the causal associations between ADHD, ASD, TS and an elevated genetic predisposition to fractures in diverse anatomical regions.
Methods
Data source for NDDs
The genomic association data for ADHD [29], ASD [30], TS [31] utilized in this study were extracted from the PGC database. The genomic association data for intelligence [32] were extracted from Complex Trait Genetics Lab (CTG) (https://ctg.cncr.nl/).
The Population Characteristics:
All participants included in the study were of European descent. The diagnostic criteria for ADHD and ASD were based on the ICD-10 (International Classification of Diseases, 10th Revision), while the diagnostic criteria for Tourette Disorder adhered to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition).
Instrumental Variables (IVs):
The IVs employed in the analysis consisted of a total of 582 SNPs. These SNPs were meticulously selected based on specific criteria, including a significance threshold of p < 5 × 10^-6, minimal linkage disequilibrium (LD) interlocking imbalance (LD r^2 < 0.001), and a clumping distance exceeding 10,000 kilobases. Detailed information about these IVs can be found in Supplementary Table.
Data source for fractures and osteoporosis
The data related to fractures and osteoporosis in this study were sourced from the FinnGen project [33], specifically utilizing the R9 version of the data, which was published on May 11, 2023. Detailed instructions and information about this research project and its data sources are available on the project’s website: FinnGen Project Information.
Diagnostic Criteria and Participant Characteristics:
The diagnosis of fractures and osteoporosis across these categories was based on the ICD-10. All individuals included in the study were of European descent.
Instrumental Variables (IVs):
IVs comprised a total of 269 SNPs. These SNPs were carefully selected based on specific criteria, including a significance threshold of p < 5 × 10^-6, minimal LD interlocking imbalance (LD r^2 < 0.001), and a clumping distance exceeding 10,000 kilobases. Comprehensive information regarding these IVs can be found in Supplementary Table.
The Details of cohort specifics of NDDs and Fractures and Osteoporosis are presented in Table 1.
Confounding factors
Numerous studies have highlighted a significant connection between early life-related traits and the emergence of neurological and psychiatric disorders in adulthood, potentially due to increased oxidative stress within the central nervous system during early life [34]. For example, a well-documented association exists between low birth weight and ADHD [35]. Additionally, the mounting prevalence of childhood obesity has emerged as a significant public health concern due to its intricate and multifaceted relationship with neurodevelopmental health challenges in adulthood [36]. Furthermore, it is worth mentioning that allergic diseases during childhood hold the potential to precipitate ADHD symptoms [37].
Management of Confounding Factors:
Moreover, existing literature has indicated that the intake of vitamin D [38], calcium [39], and zinc [40] serve as risk factors for fractures and osteoporosis. Supplementation with vitamin D has been shown to augment bone density, thereby mitigating the risks of fractures and osteoporosis [38]. Calcium and vitamin D have been identified as pivotal determinants of peak bone mass [39]. Conversely, a diminished intake of zinc is associated with an elevated risk of fractures and osteoporosis [40]. Consequently, we have incorporated dietary supplements of vitamin D, calcium, and zinc as confounding variables in this study.
In light of the aforementioned considerations, this study rigorously controlled for potential confounding factors. It incorporated birth height [41], birth weight [42], body mass index (BMI) [43], and the presence of allergic diseases within the analytical framework. The impact of these factors on the observed outcomes was meticulously addressed by excluding SNPs that showed overlap within the IVs. Birth height, weight, and children’s BMI data were sourced from The Early Growth Genetics (EGG) Consortium, while information on allergic diseases was acquired from a Finnish database [33]. The data on theintakeof vitamin D, calcium, and zinc were sourced from the IEU Open GWAS database [44]. This comprehensive approach enhances the study’s robustness, minimizing the influence of potential confounders and bolstering the precision of causal inferences.
Statistical analysis
This study employed a MR approach to explore the intricate bidirectional relationship between ADHD, ASD, TS, and 11 distinct types of fractures and osteoporosis.
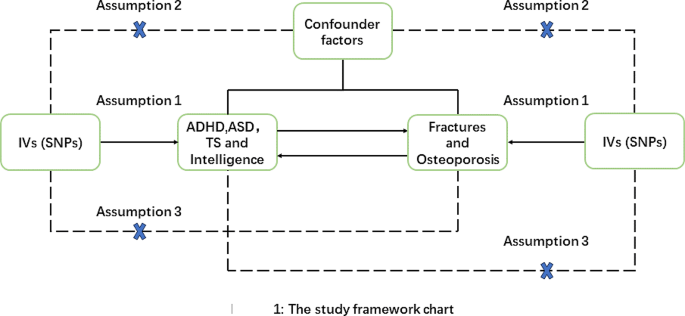
The study adhered to the classical MR assumptions (Fig. 1)
MR assumptions and design of our study:1. IV Exposure Association: IVs demonstrated a robust association with the exposure of interest.2. Absence of Unidentified Confounding: IVs were selected to have no associations with unidentified confounding factors that could affect both the exposure and outcome.3. IV Effect via Exposure: IVs exclusively influenced the outcomes through the exposure under investigation
To mitigate confounding factors, the study rigorously screened IVs and established a significance threshold (P < 5e-06) to minimize weak associations between potential confounders and genetic variations.
The primary statistical metric used was the inverse variance weighted (IVW) method, assessing the association between ADHD, ASD, and fractures or osteoporosis. MR-Egger, weighted median, and weighted models served as supplementary statistical indicators.
Sensitivity analysis, a crucial component of MR analysis, was employed to detect potential pleiotropy. Heterogeneity was assessed using the Cochrane Q test, and horizontal pleiotropy was examined via the MR-Egger intercept method. A leave-one-out analysis assessed the impact of individual SNPs on MR results. In cases of heterogeneity, the random-effect IVW was used as the primary statistical measure, while the fixed-effect IVW was employed when no heterogeneity was observed.
The significance threshold for results was corrected for multiple testing using the Bonferroni method. A p-value of < 0.001 (0.05/36) was considered significant, p-values between 0.001 and 0.05 were considered suggestive, and p-values above 0.05 were deemed insignificant. The F statistic \( (F=\frac{bet{a}^{2}}{s{e}^{2}})\) was used to assess the strength of IVs, with F > 10 indicating a robust and independent instrumental variable [45].
All statistical analyses were performed using the TwoSample MR package in R version 4.2.2, and the results were reported in terms of odds ratio (OR) values with associated 95% confidence intervals.
Result
Causal relationship between fractures and osteoporosis and ADHD, ASD, TS and intelligence
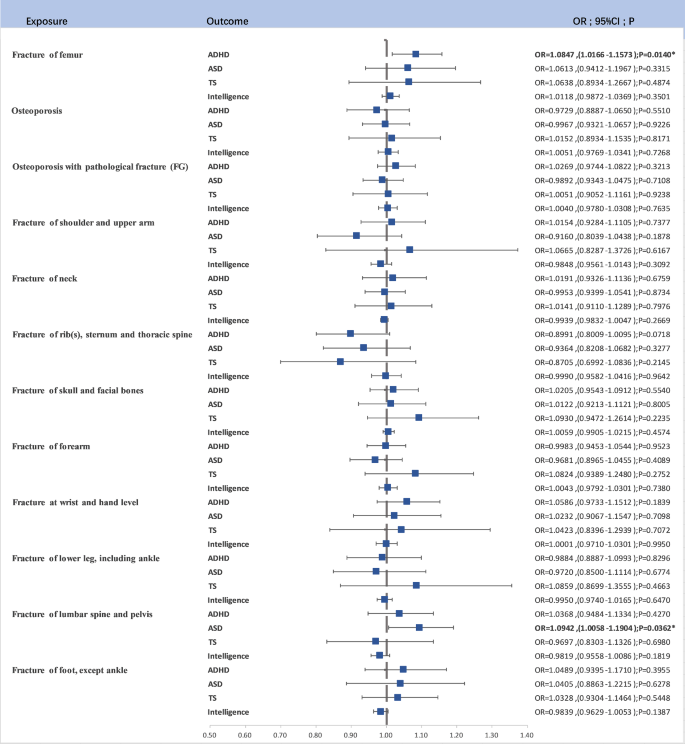
A similar screening process, accounting for P-values and LD clumping, was applied to SNPs used as IVs for different fracture and osteoporosis outcomes. Although potential causal relationships were detected, they did not consistently reach statistical significance after Bonferroni correction (Fig. 2)
Fracture of femur and ADHD: A suggestive causal relationship was observed (OR = 1.0847, 95% CI (1.0166–1.1573), P = 0.0140).
Fracture of lumbar spine and pelvis and ASD: Another suggestive causal relationship was noted (OR = 1.0942, 95% CI (1.0058–1.1904), P = 0.0362).
These findings, while suggestive, did not maintain statistical significance following Bonferroni correction but offer valuable insights into potential risk factors.
Heterogeneity and Pleiotropy Testing:
Detailed information on the results of heterogeneity and pleiotropy testing is available in the supplementary material and supplementary table, providing a comprehensive assessment of the findings’ robustness in light of these factors.
Causal relationship between ADHD, ASD, TS, intelligence and fracture risk
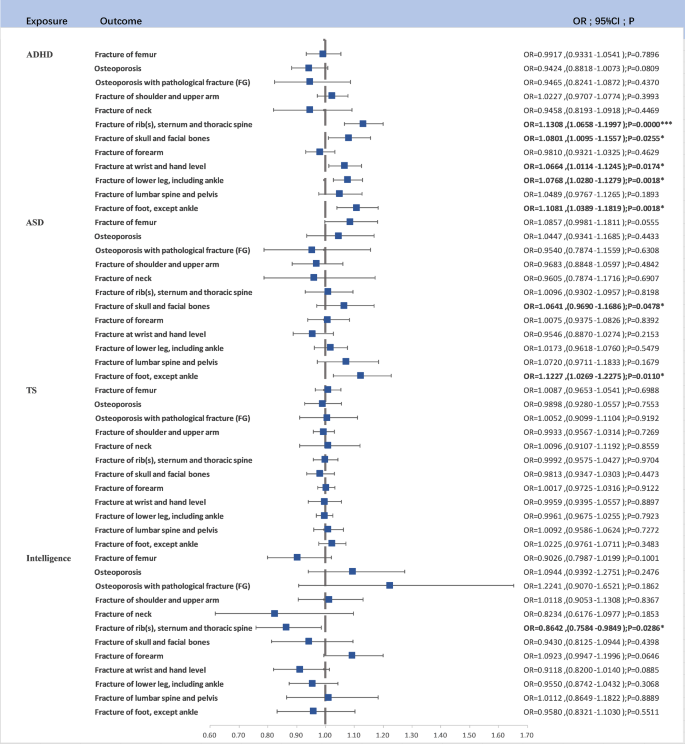
After rigorous SNP screening based on P-values and LD clumping, a total of 138, 34, 22 and 387 linkage-disequilibrium-independent SNPs served as IVs for ADHD, ASD, TS and Intelligence. Upon eliminating SNPs not present in the outcome variable, a two-sample MR analysis unveiled significant findings (Fig. 3).
ADHD as a Risk Factor: ADHD was identified as a risk factor for Fracture of rib(s), sternum, and thoracic spine (OR = 1.1308, 95% CI (1.0658–1.1997), P < 0.0001). This association retained significance after Bonferroni correction. ADHD was also linked to Fracture of foot (except ankle) (OR = 1.1081, 95% CI (1.0389–1.1819), P = 0.0018), Fracture of lower leg (including ankle) (OR = 1.0768, 95% CI (1.0280–1.1279), P = 0.0018), Fracture at wrist and hand level (OR = 1.0664, 95% CI (1.0114–1.1245), P = 0.0174), and Fracture of skull and facial bones (OR = 1.0801, 95% CI (1.0095–1.1557), P = 0.0255).
ASD as a Risk Factor: ASD was found to be associated with an increased risk of Fracture of foot (except ankle) (OR = 1.1227, 95% CI (1.0269–1.2275), P = 0.0110).
TS as a Risk Factor: No significant causal relationship wasfoundin TS.
Additionally, we observed that higher levels of intelligence were associated with a reduced risk of fractures involving the rib(s), sternum, and thoracic spine (OR = 0.8642, 95% CI (0.7584–0.9849), P = 0.0286). The pleiotropy and heterogeneity test results are included in the supplementary materials.
Discussion
This comprehensive study adopted a bidirectional MR approach to investigate the intricate relationships between three NDDs—ADHD, ASD, and TS—and a spectrum of 11 distinct fractures and osteoporosis. The MR analysis provided intriguing insights into these associations, shedding light on potential causal links and risk factors (Fig. 4).
Fractures as causal factors
The MR analysis results suggested that certain fractures may act as causal factors in the development of these childhood NDDs. Specifically, a fracture of the femur may be a risk factor for ADHD (P = 0.0140), and fractures of the lumbar spine and pelvis may be risk factors for ASD (P = 0.0362). Although these findings did not retain statistical significance after Bonferroni correction, they offer valuable indications of potential associations.
NDDs as causal factors
Conversely, the reverse MR analysis presented robust findings indicating that ADHD could be a causal factor for various types of fractures. For example, ADHD is a risk factor for fractures of the rib(s), sternum, and thoracic spine (P < 0.0001), fractures of the foot (except ankle) (P = 0.0018), fractures of the lower leg (including ankle) (P = 0.0003), fractures at the wrist and hand level (P = 0.0174), and fractures of the craniofacial region (P = 0.0255). Similarly, ASD is considered a risk factor for foot fractures (P = 0.0110), and higher intelligence levels are associated with a preventive effect against the occurrence of fractures involving the rib(s), sternum, and thoracic spine (P = 0.0286). Besides, there is no causal relationship between fractures and TS.
Observational studies have historically grappled with the intricate connections among ADHD, ASD, TS, and fractures, as well as osteoporosis. Often, symptoms linked to these NDDs may unintentionally escape attention when investigating fractures [46]. Our study represents a pioneering effort, constituting the inaugural systematic exploration of the link between childhood NDDs and fractures and osteoporosis through a genetic framework. By adeptly sidestepping potential confounding variables, measurement inaccuracies, and other sources of bias, the study yields invaluable genetic insights. Significantly, it identifies NDDs like ADHD as potential contributors to various fractures, while also suggesting that fractures might be potential causes of diverse fractures. However, this perspective requires further research for clarification. It introduces a new perspective on the potential interplay between psychological well-being and bone health.
Fractures not only induce pain and inflammatory reactions but recent research has also uncovered connections between NDDs and pain [47, 48]. Interestingly, the prevalence of ADHD is significantly higher in adolescents experiencing chronic pain [49,50,51], and inflammation is suggested as a contributing factor in the development of ADHD and ASD [52, 53]. For instance, inflammatory pain in newborns and responses in preterm infants may elevate the risk of NDDs [54]. In individuals with ADHD, elevated levels of inflammatory biomarkers and inflammation within the central nervous system are believed to contribute to pain perception and sensitization [54, 55]. This also holds promise for preventing chronic pain in adults with ADHD through neuroinflammation treatment [56].
Shifting focus to the post-traumatic inflammatory response, microglia and their associated molecular pathways play a pivotal role [57], especially in scenarios like traumatic brain injury (TBI) [58]. Research indicates that TBI coincides with heightened neuroinflammatory responses, as observed in mice with tibial fractures [59]. These responses are concurrent with disruptions in the blood-brain barrier and behavioral deficits. The increase in interleukin-1β (IL-1β) levels in the brain is associated with these changes, influencing astrocytes, microglia, and neurons while governing neuroinflammatory processes [57, 60]. This series of findings underscores the intricate interplay among fractures, NDDs, inflammation, and pain.
Vitamin D is crucial for both musculoskeletal well-being and brain function. It is indispensable for maintaining healthy bones, but its deficiency can elevate the risk of fractures [61, 62]. In terms of brain function, vitamin D functions as a neurosteroid hormone, influencing neurodevelopment processes such as nerve cell proliferation, neurotransmission, oxidative stress regulation, and immune function—all of which are integral to the central nervous system [63, 64].
Vitamin D deficiency has been linked to various NDDs and psychiatric disorders, including ADHD, ASD, and schizophrenia [65,66,67]. Individuals with ADHD and ASD frequently exhibit lower levels of 25-hydroxyvitamin D (25(OH)D) in their serum compared to their healthy counterparts [68, 69]. Moreover, an inverse relationship exists between vitamin D and its receptor levels (VDR) and the severity of ASD and ADHD [70, 71]. This suggests that vitamin D may play a significant role not only in the development of ASD but also in ADHD and fractures.
In the context of ASD, children typically engage in less physical activity, have a lower BMI, and may not consume adequate amounts of calcium and calories [72, 73]. These factors collectively increase the risk of low bone density in individuals with ASD [15, 74]. For ADHD, various factors contribute to injuries and fractures in affected children. Some of these incidents can be attributed to the unique characteristics of ADHD [75]. Impulsivity is a hallmark symptom of ADHD, characterized by actions taken without prior thought, insufficient judgment, and a tendency to seek immediate gratification [10, 75]. Research suggests that children with ADHD, despite being capable of recognizing dangers, tend to underestimate the severity of consequences arising from their behaviors [76]. This inherent impulsivity may render children with ADHD more susceptible to injuries and fractures, even in situations comparable to their peers without ADHD [75]. Similarly, low intelligence in the early years has been shown to increase the risk of unintentional injury [77].
However, it is crucial to acknowledge certain limitations in our study. Firstly, we did not analyze the causal relationship between ADHD, ASD, and fractures based on variables such as sex, age, BMI, and other relevant factors. Nevertheless, existing research suggests that these factors could potentially influence causation. Secondly, our study exclusively relied on genetic data from individuals of European ancestry, and we did not validate our findings in non-European populations. As a result, the generalizability of our conclusions to non-European populations remains uncertain.
While our study has several important strengths, providing insights into healthcare management strategies for children with ADHD, it is essential to recognize its limitations. Our findings emphasize the importance of prioritizing the bone health of children with ADHD by monitoring their BMD and implementing appropriate vitamin D supplementation strategies. Furthermore, our results may prompt a shift in the approach to fractures in children. ADHD symptoms are often overlooked in the context of fracture management, and our study aims to address this gap. One key strength of our research lies in the application of the MR method. This approach effectively addresses the potential influence of external social factors on the relationship between exposure variables and outcomes, thereby enhancing the robustness and reliability of our findings.
Data availability
Summary data on ADHD, ASD, TS, Fractures and Osteoporosis is available on supplementary material.
References
Jain P, Miller-Fleming T, Topaloudi A, Yu D, Drineas P, Georgitsi M, Yang Z, Rizzo R, Müller-Vahl KR, Tumer Z et al. Polygenic risk score-based phenome-wide association study identifies novel associations for Tourette syndrome. Translational Psychiatry 2023, 13(1).
Whitney DG, Caird MS, Jepsen KJ, Kamdar NS, Marsack-Topolewski CN, Hurvitz EA, Peterson MD. Elevated fracture risk for adults with neurodevelopmental disabilities. Bone 2020, 130.
Chou IC, Lin CC, Sung FC, Kao CH. Attention-deficit‐hyperactivity disorder increases risk of bone fracture: a population‐based cohort study. Dev Med Child Neurol. 2014;56(11):1111–6.
Perry BA, Archer KR, Song Y, Ma Y, Green JK, Elefteriou F, Dahir KM. Medication therapy for attention deficit/hyperactivity disorder is associated with lower risk of fracture: a retrospective cohort study. Osteoporos Int. 2016;27(7):2223–7.
Guo N-W, Lin C-L, Lin C-W, Huang M-T, Chang W-L, Lu T-H, Lin C-J. Fracture risk and correlating factors of a pediatric population with attention deficit hyperactivity disorder: a nationwide matched study. J Pediatr Orthop B. 2016;25(4):369–74.
Prasad V, West J, Sayal K, Kendrick D. Injury among children and young people with and without attention-deficit hyperactivity disorder in the community: the risk of fractures, thermal injuries, and poisonings. Child Care Health Dev. 2018;44(6):871–8.
Merrill RM, Lyon JL, Baker RK, Gren LH. Attention deficit hyperactivity disorder and increased risk of injury. Adv Med Sci. 2009;54(1):20–6.
Kömürcü E, Bilgiç A, Hergüner S. Relationship between extremity fractures and attention-deficit/hyperactivity disorder symptomatology in adults. Int J Psychiatry Med. 2014;47(1):55–63.
Jacob L, Kostev K. Impact of attention deficit hyperactivity disorder therapy on fracture risk in children treated in German pediatric practices. Osteoporos Int. 2017;28(4):1265–9.
Ziv-Baran T, Zacay G, Modan-Moses D, Reingold SM, Mekori E, Levy-Shraga Y. Increased fracture risk among children diagnosed with attention- deficit/hyperactivity disorder: a large matched cohort study. Eur J Pediatrics. 2023;182(6):2705–14.
Hashem S, Nisar S, Bhat AA, Yadav SK, Azeem MW, Bagga P, Fakhro K, Reddy R, Frenneaux MP, Haris M. Genetics of structural and functional brain changes in autism spectrum disorder. Translational Psychiatry 2020, 10(1).
McDermott S, Zhou L, Mann J. Injury Treatment among children with autism or pervasive developmental disorder. J Autism Dev Disord. 2007;38(4):626–33.
Neumeyer AM, O’Rourke JA, Massa A, Lee H, Lawson EA, McDougle CJ, Misra M. Brief report: bone fractures in children and adults with Autism Spectrum disorders. J Autism Dev Disord. 2014;45(3):881–7.
Ekhlaspour L, Baskaran C, Campoverde KJ, Sokoloff NC, Neumeyer AM, Misra M. Bone density in adolescents and young adults with Autism Spectrum disorders. J Autism Dev Disord. 2016;46(11):3387–91.
Rostami Haji Abadi M, Neumeyer A, Misra M, Kontulainen S. Bone health in children and youth with ASD: a systematic review and meta-analysis. Osteoporos Int. 2021;32(9):1679–91.
Lu Y-Y, Wang M-Y, Wei IH, Lin C-C, Huang C-C. Tourette syndrome increases risk of bone fractures: a population-based cohort study. Eur Child Adolesc Psychiatry. 2016;26(5):531–9.
Armenteros JL, Davies M. Antipsychotics in early onset Schizophrenia. Eur Child Adolesc Psychiatry. 2006;15(3):141–8.
Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359(9321):1929–36.
Wilson-Barnes SL, Lanham-New SA, Lambert H. Modifiable risk factors for bone health & fragility fractures. Best Pract Res Clin Rheumatol 2022, 36(3).
Boudin E, Fijalkowski I, Hendrickx G, Van Hul W. Genetic control of bone mass. Mol Cell Endocrinol. 2016;432:3–13.
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R. Clinician’s guide to Prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359–81.
Denova-Gutiérrez E, Méndez-Sánchez L, Muñoz-Aguirre P, Tucker KL, Clark P. Dietary patterns, bone Mineral Density, and risk of fractures: a systematic review and Meta-analysis. Nutrients 2018, 10(12).
Lane JC, Butler KL, Poveda-Marina JL, Martinez-Laguna D, Reyes C, de Bont J, Javaid MK, Logue J, Compston JE, Cooper C, et al. Preschool obesity is Associated with an increased risk of Childhood fracture: a longitudinal cohort study of 466,997 children and up to 11years of follow-up in Catalonia, Spain. J Bone Min Res. 2020;35(6):1022–30.
Jia N, Dong L, Lu Q, Li X, Jin M, Yin X, Zhu Z, Jia Q, Ji C, Hui L, et al. The causal effect of schizophrenia on fractures and bone mineral density: a comprehensive two-sample mendelian randomization study of European ancestry. BMC Psychiatry. 2023;23(1):692.
Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. In: Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc. 2013: xliv, 947-xliv, 947.
Åsberg Johnels J, Yngvesson P, Billstedt E, Gillberg C, Halldner L, Råstam M, Gustafsson P, Selinus EN, Lichtenstein P, Hellner C, et al. The relationship between intelligence and global adaptive functioning in young people with or without neurodevelopmental disorders. Psychiatry Res. 2021;303:114076.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89–98.
Richmond RC, Anderson EL, Dashti HS, Jones SE, Lane JM, Strand LB, Brumpton B, Rutter MK, Wood AR, Straif K et al. Investigating causal relations between sleep traits and risk of breast cancer in women: mendelian randomisation study. BMJ 2019.
Demontis D, Walters GB, Athanasiadis G, Walters R, Therrien K, Nielsen TT, Farajzadeh L, Voloudakis G, Bendl J, Zeng B, et al. Genome-wide analyses of ADHD identify 27 risk loci, refine the genetic architecture and implicate several cognitive domains. Nat Genet. 2023;55(2):198–208.
Grove J, Ripke S, Als TD, Mattheisen M, Walters RK, Won H, Pallesen J, Agerbo E, Andreassen OA, Anney R, et al. Identification of common genetic risk variants for autism spectrum disorder. Nat Genet. 2019;51(3):431–44.
Yu D, Sul JH, Tsetsos F, Nawaz MS, Huang AY, Zelaya I, Illmann C, Osiecki L, Darrow SM, Hirschtritt ME, et al. Interrogating the genetic determinants of Tourette’s syndrome and other Tic disorders through genome-wide Association studies. Am J Psychiatry. 2019;176(3):217–27.
Savage JE, Jansen PR, Stringer S, Watanabe K, Bryois J, de Leeuw CA, Nagel M, Awasthi S, Barr PB, Coleman JRI, et al. Genome-wide association meta-analysis in 269,867 individuals identifies new genetic and functional links to intelligence. Nat Genet. 2018;50(7):912–9.
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner KM, Reeve MP, Laivuori H, Aavikko M, Kaunisto MA, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613(7944):508–18.
Schiavone S, Colaianna M, Curtis L. Impact of early life stress on the Pathogenesis of Mental disorders: relation to Brain oxidative stress. Curr Pharm Design. 2015;21(11):1404–12.
Momany AM, Kamradt JM, Nikolas MA. A Meta-analysis of the Association between Birth Weight and attention deficit hyperactivity disorder. J Abnorm Child Psychol. 2018;46(7):1409–26.
He R, Mo J, Zhu K, Luo Q, Liu X, Huang H, Sheng J. The early life course-related traits with three psychiatric disorders: a two-sample mendelian randomization study. Front Psychiatry 2023, 14.
Xu X, Zhuo L, Zhang L, Peng H, Lyu Y, Sun H, Zhai Y, Luo D, Wang X, Li X, et al. Dexmedetomidine alleviates host ADHD-like behaviors by reshaping the gut microbiota and reducing gut-brain inflammation. Psychiatry Res. 2023;323:115172.
Lips P, van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab. 2011;25(4):585–91.
Vannucci L, Masi L, Gronchi G, Fossi C, Carossino AM, Brandi ML. Calcium intake, bone mineral density, and fragility fractures: evidence from an Italian outpatient population. Archives Osteoporos 2017, 12(1).
Ceylan MN, Akdas S, Yazihan N. Is zinc an important Trace element on bone-related diseases and complications? A Meta-analysis and systematic review from serum level, Dietary Intake, and supplementation aspects. Biol Trace Elem Res. 2020;199(2):535–49.
van der Valk RJP, Kreiner-Møller E, Kooijman MN, Guxens M, Stergiakouli E, Sääf A, Bradfield JP, Geller F, Hayes MG, Cousminer DL, et al. A novel common variant in DCST2 is associated with length in early life and height in adulthood. Hum Mol Genet. 2015;24(4):1155–68.
Warrington NM, Beaumont RN, Horikoshi M, Day FR, Helgeland Ø, Laurin C, Bacelis J, Peng S, Hao K, Feenstra B, et al. Maternal and fetal genetic effects on birth weight and their relevance to cardio-metabolic risk factors. Nat Genet. 2019;51(5):804–14.
Copenhaver GP, Vogelezang S, Bradfield JP, Ahluwalia TS, Curtin JA, Lakka TA, Grarup N, Scholz M, van der Most PJ, Monnereau C et al. Novel loci for childhood body mass index and shared heritability with adult cardiometabolic traits. PLoS Genet 2020, 16(10).
Elsworth B, Lyon M, Alexander T, Liu Y, Matthews P, Hallett J, Bates P, Palmer T, Haberland V, Smith GD et al. The MRC IEU OpenGWAS data infrastructure. 2020:2020.2008.2010.244293.
Yao C, Zhang Y, Lu P, Xiao B, Sun P, Tao J, Cheng Y, Kong L, Xu D, Fang M. Exploring the bidirectional relationship between pain and mental disorders: a comprehensive mendelian randomization study. J Headache Pain 2023, 24(1).
Davison R, Daniel JA, Idarraga AJ, Perticone KM, Lin J, Holmes GB, Lee S, Hamid KS, Bohl DD. Depression following operative treatments for Achilles ruptures and Ankle fractures. Foot Ankle Int. 2021;42(12):1579–83.
Low Kapalu CM, Hall JJ, Wallace DP. Neuropsychological functioning of Youth receiving Intensive Interdisciplinary Pain Treatment. J Pediatr Psychol. 2018;43(8):870–81.
Battison E, Brown P, Holley A, Wilson A. Associations between Chronic Pain and attention-deficit hyperactivity disorder (ADHD) in youth: a scoping review. Children 2023, 10(1).
Hechler T, Kanstrup M, Holley AL, Simons LE, Wicksell R, Hirschfeld G, Zernikow B. Systematic review on Intensive Interdisciplinary Pain Treatment of Children with Chronic Pain. Pediatrics. 2015;136(1):115–27.
Wiwe Lipsker C, von Heijne M, Bölte S, Wicksell RK. A case report and literature review of autism and attention deficit hyperactivity disorder in paediatric chronic pain. Acta Paediatr. 2018;107(5):753–8.
Wiwe Lipsker C, Bölte S, Hirvikoski T, Lekander M, Holmström L, Wicksell RK. Prevalence of autism traits and attention-deficit hyperactivity disorder symptoms in a clinical sample of children and adolescents with chronic pain. J Pain Res. 2018;11:2827–36.
Bryn V, Aass HC, Skjeldal OH, Isaksen J, Saugstad OD, Ormstad H. Cytokine Profile in Autism Spectrum disorders in Children. J Mol Neurosci. 2017;61(1):1–7.
Anand D, Colpo GD, Zeni G, Zeni CP, Teixeira AL. Attention-Deficit/Hyperactivity disorder and inflammation: what does current knowledge tell us? A systematic review. Front Psychiatry 2017, 8.
Lee JH, Espinera AR, Chen D, Choi K-E, Caslin AY, Won S, Pecoraro V, Xu G-Y, Wei L, Yu SP. Neonatal inflammatory pain and systemic inflammatory responses as possible environmental factors in the development of autism spectrum disorder of juvenile rats. J Neuroinflamm 2016, 13(1).
Koç S, Güler EM, Derin S, Gültekin F, Aktaş S. Oxidative and inflammatory parameters in children and adolescents with ADHD. J Atten Disord. 2023;27(8):880–6.
Kerekes N, Sanchéz-Pérez AM, Landry M. Neuroinflammation as a possible link between attention-deficit/hyperactivity disorder (ADHD) and pain. Med Hypotheses. 2021;157:110717.
Prata J, Santos SG, Almeida MI, Coelho R, Barbosa MA. Bridging Autism Spectrum disorders and Schizophrenia through inflammation and biomarkers - pre-clinical and clinical investigations. J Neuroinflamm 2017, 14(1).
Urrutia-Ruiz C, Rombach D, Cursano S, Gerlach-Arbeiter S, Schoen M, Bockmann J, Demestre M, Boeckers TM. Deletion of the Autism-Associated protein SHANK3 abolishes structural synaptic plasticity after Brain Trauma. Int J Mol Sci 2022, 23(11).
Lu S-M, Yu C-J, Liu Y-H, Dong H-Q, Zhang X, Zhang S-S, Hu L-Q, Zhang F, Qian Y-N, Gui B. S100A8 contributes to postoperative cognitive dysfunction in mice undergoing tibial fracture surgery by activating the TLR4/MyD88 pathway. Brain Behav Immun. 2015;44:221–34.
Pike AF, Varanita T, Herrebout MAC, Plug BC, Kole J, Musters RJP, Teunissen CE, Hoozemans JJM, Bubacco L, Veerhuis R. α-Synuclein evokes NLRP3 inflammasome‐mediated IL‐1β secretion from primary human microglia. Glia. 2021;69(6):1413–28.
Silva ICJ, Lazaretti-Castro M. Vitamin D metabolism and extraskeletal outcomes: an update. Archives Endocrinol Metabolism. 2022;66(5):748–55.
Dixon KM, Mason RS. Vitamin D. Int J Biochem Cell Biol. 2009;41(5):982–5.
Rihal V, khan H, Kaur A, Singh TG, Abdel-Daim MM. Therapeutic and mechanistic intervention of vitamin D in neuropsychiatric disorders. Psychiatry Res. 2022;317:114782.
Ali A, Cui X, Eyles D. Developmental vitamin D deficiency and autism: putative pathogenic mechanisms. J Steroid Biochem Mol Biol. 2018;175:108–18.
Ye X, Zhou Q, Ren P, Xiang W, Xiao L. The Synaptic and Circuit Functions of Vitamin D in Neurodevelopment disorders. Neuropsychiatr Dis Treat. 2023;19:1515–30.
Gáll Z, Székely O. Role of vitamin D in cognitive dysfunction: new molecular concepts and discrepancies between animal and human findings. Nutrients. 2021;13(11):3672.
Siracusano M, Riccioni A, Abate R, Benvenuto A, Curatolo P, Mazzone L. Vitamin D Deficiency and Autism Spectrum Disorder. Curr Pharm Design. 2020;26(21):2460–74.
Kotsi E, Kotsi E, Perrea DN. Vitamin D levels in children and adolescents with attention-deficit hyperactivity disorder (ADHD): a meta-analysis. ADHD Atten Deficit Hyperactivity Disorders. 2019;11(3):221–32.
Saedisomeolia A, Samadi M, Gholami F, Seyedi M, Effatpanah M, Hashemi R, Abdolahi M, Honarvar MN. Vitamin D’s molecular action mechanism in Attention-Deficit/ hyperactivity disorder: a review of evidence. CNS Neurol Disorders - Drug Targets. 2018;17(4):280–90.
Ogbu D, Xia E, Sun J. Gut instincts: vitamin D/vitamin D receptor and microbiome in neurodevelopment disorders. Open Biology 2020, 10(7).
Ganta A, Pillai SS, Fredette ME, Topor LS. Severe Vitamin D Deficiency in Youth with Autism Spectrum Disorder during the COVID-19 pandemic. J Dev Behav Pediatr. 2022;43(8):461–4.
Gehricke J-G, Chan J, Farmer JG, Fenning RM, Steinberg-Epstein R, Misra M, Parker RA, Neumeyer AM. Physical activity rates in children and adolescents with autism spectrum disorder compared to the general population. Res Autism Spectr Disorders 2020, 70.
Soden SE, Garrison CB, Egan AM, Beckwith AM. Nutrition, Physical Activity, and bone Mineral Density in Youth with Autistic Spectrum disorders. J Dev Behav Pediatr. 2012;33(8):618–24.
Calarge CA, Schlechte JA. Bone Mass in boys with Autism Spectrum Disorder. J Autism Dev Disord. 2017;47(6):1749–55.
Seens H, Modarresi S, MacDermid JC, Walton DM, Grewal R. Prevalence of bone fractures among children and adolescents with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. BMC Pediatr. 2021;21(1):354.
Farmer JE, Peterson L. Injury risk factors in children with attention deficit hyperactivity disorder. Health Psychol. 1995;14(4):325–32.
Whitley E, Batty GD, Gale CR, Deary IJ, Tynelius P, Rasmussen F. Intelligence in early adulthood and subsequent risk of unintentional injury over two decades: cohort study of 1 109 475 Swedish men. J Epidemiol Community Health. 2009;64(5):419–25.
Acknowledgements
We want to acknowledge the participants and investigatorsof the FinnGen, UK Biobank, Psychiatric GenomicsConsortium (PGC), The Early Growth Genetics(EGG) study
Funding
This research was supported by Jinan City’s “20 Colleges and Universities” funded project.
(No. 2020GXRC013); National Administration of Traditional Chinese Medicine Project(GZY-KJS-2023-017); Qingdao Science and Technology Benefiting the People Demonstration Special Project(23-7-8-smjk-3-nsh).
Author information
Authors and Affiliations
Contributions
Xueqiang Wu and Zefang Li: conceptualization and writing-original draft. Hanzheng Li, Cong Bi, Can Zhang and Yiqing Sun: data curation and formal analysis. Zhaojun Yan funding acquisition and validation. Xueqiang Wu and Zhaojun Yan: methodology. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
Supplementary Material Supplementary Figure 1, 4, 7, 10 and 10-22 showed the leave one out plot of NDDs on bone fractures and osteoporosis; Figure 2, 5, 8 and 22 showed the funnel plot of NDDs on bone fractures and osteoporosis; Figure 3, 6, 9 and 23 showed the scatter plot of NDDs on bone fractures and osteoporosis. Supplementary Figure 24-26 showed the leave one out plot bone fractures and osteoporosis on NDDs; Supplementary Figure 27-29 showed the funnel plot bone fractures and osteoporosis on NDDs; Supplementary Figure 30-32 showed the scatter plot bone fractures and osteoporosis on NDDs
Supplementary Material 2:
Table S1, Summary data for exposure and outcome; Table S2, The IVs for our study; Table S3, The results for causal effect; Table S4, Results of heterogeneity test; Table S5, Results of sensitivity analysis
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Z., Wu, X., Li, H. et al. Complex interplay of neurodevelopmental disorders (NDDs), fractures, and osteoporosis: a mendelian randomization study. BMC Psychiatry 24, 232 (2024). https://doi.org/10.1186/s12888-024-05693-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05693-4